introduction to human physiology
Introduction To Human Physiology
- Respiratory system is the system responsible for equipment of air to the body tissues.
- Respiration is a complex process by which living organisms exchange O2 and CO2 between the organism and the environment.
- Respiration is important in obtaining energy by oxidation of food substances. The obtained energy is stored in form of high energy phosphate compounds like ATP.
- Respiration includes many processes:
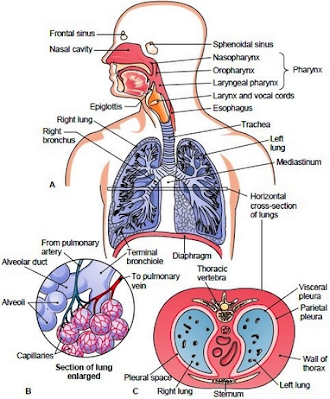
- Trachea the first generation respiratory passageway is divided into right and left main bronchi, which are the second generation respiratory passageway.
- Bronchus in turn is divided into small branches: the bronchioles inside the lung.
- Bronchioles are further divided into very small bronchioles: the respiratory bronchioles.
- There are 20- 25 generations before reaching finally to the alveolar duct and alveoli.
- The inner surface of the trachea (bronchi and bronchioles) is lined with mucus secreting goblet cells (the mucus traps foreign particles, e.g. dust and parasites) and ciliated cells carrying the mucus to the nose .
- Conducting zone extend from the trachea to terminal bronchioles which are ciliated for removal of debris. It is anatomically incapable of gas exchange but they work as a passageway for air movement. It constitutes the anatomical dead space.
- Respiratory zone extends from the respiratory bronchioles to the alveoli. It is a site for gas exchange.
- Lungs are principle organs of the respiratory system. Each lung is conical shape resting on the diaphragm.
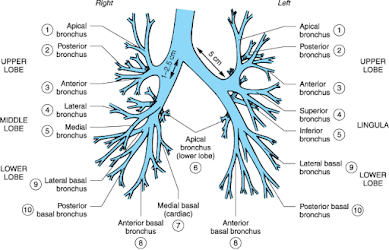
- The right lung is larger than the left lung. The right lung has three lobes while the left lung has two lobes .Each lobe is supplied by a lobar bronchus. The lobes are divided into bronchopulmonary segments which are supplied by the segmental bronchi - Nine bronchopulmonary segments are present in the left lung. - Ten bronchopulmonary segments are present in the right lung.
- The lung is surrounded by a double layered serous membrane called pleura:
- - Parietal pleura is the outer layer of the pleura - Visceral pleura are the inner layer, directly connected to the lung. - Pleural cavity – slit-like potential space filled with 2 ml mucoid pleural fluid, which is secreted by parietal pleura;
- Function of the pleural fluid:
- Pulmonary ventilation means inflow and outflow of air between the atmosphere and the lung alveoli.
- Air moves from the region of a high pressure to one of a lower pressure.
- A pressure difference is established by the mechanics of pulmonary ventilation: inspiration and expiration.
- The muscles cause the lungs to expand and contract.
- Lungs can be expanded and contracted in two ways:
- Inspiration is an active process.
- The dome shaped diaphragm flattens as it contracts. This increases the height of the thoracic cavity.
- The external intercostal muscles contract to raise the ribs .This increases the circumference of the thoracic cavity
- During deep or forced inspiration, additional muscles are recruited: scalene, sternocleidomastoid and pectoralis minor.
- Intrapleural pressure becomes more negative (-2.5 − -6)mmHg ,due to increase thoracic volume ,as compare to the atmospheric pressure, therefore air flows into the lung.
- Quiet expiration in healthy people is a passive process(no muscle contraction)
- Inspiratory muscles relax .
- Relaxing diaphragm moves superiorly (up).
- Elastic fibers in lung recoil
- Volumes of thorax and lungs decrease simultaneously, increasing the pressure to slightly positive so the air flows out of the lungs.
- Expiration during the exercise or lung diseases becomes active process requiring use of accessory muscles like internal intercostal muscles and abdominal muscles.
- The lungs have tendency to collapse due to their elastic structures, therefore they collapse like a balloon to expel the air through the trachea when there is no force to keep it inflated.
- The lung floats in the thoracic cavity surrounded by pleural fluid that lubricates movement of the lung in the thoracic cavity.
Dalton‟s law:
The partial The
greater the difference in partial pressure
pressure of a gas
in a mixture of between 2 points, the greater the rate of gas gases is the
percentage of the gas movement.
in the mixture times the total
pressure of the mixture of gas.
Henry‟s law:
The concentration
A small amount of the gases in air dissolves
of a gas dissolved in a liquid is in the fluid lining the alveoli (CO2 is
equal to the partial pressure of 24times more soluble than O2, therefore the
gas over the liquid times the CO2exits through the
respiratory membrane
solubility coefficient of the gas. more readily than O2 enters).
Alveolar pressure during inspiration and expiration
Work of breathing
- Work of breathing is pressure volume work performed in
moving air into and out of the lungs. Most of this work is performed during
inspiration.
- Work of breathing must overcome three sources of resistance
encountered during inspiration :
1- Airway
resistance is generated between air molecules
and the walls of conducting airways.
• Most of the total airway resistance comes from the large
conducting airways, because they are arranged in series and airflow resistances
are additive.
• Small airways provide little resistance because they
arranged in parallel and airflow resistance in parallel are added reciprocally.
Pathophysiology note: Airway diameter
can be reduced(and increased airway
resistance)by number of cases e.g., airway diameters are reduced by smooth muscle contraction and
excess inflammatory secretions in
obstructive airway diseases such as asthma and chronic bronchitis .As a result work caused by airway resistance increases
Pharmacology note: Many classes of drugs affect large airway diameter by affecting bronchial smooth muscles tone .For example β2 –adrenergic agonists such as albuterol which stimulates bronchodilation. Other classes of drugs prevent bronchoconstriction or inhibit inflammation e.g., steroids anticholinergics ,leukotriene receptors antagonists and lipoxygenase inhibitors .
2- Compliance work: is the work performed to overcome elastic recoil of the lungs. It accounts for the largest proportion of the total work of breathing.
Pathology
note: In emphysema compliance
work is reduced because the destruction of
lung tissues and loss of elastic tissues of the lung, but in pulmonary fibrosis, compliance work
is increased because the fibrotic tissues
require more work to expand.
2- Tissues resistance: is
generated as the pleural surfaces slide over each other during respiratory
cycle .It accounts for a small portion (5%) of the total work of breathing.
3-Pulmonary compliance
- Pulmonary compliance is a measure of lung dispensability.
- It is defined as the extent to which the lung will expand
for each unit increase in transpulmonary pressure. Compliant lungs are easy to
distend.
- Total lung compliance of both lungs and thorax is 200ml/cm.H2O, every time
transpulmonary pressure increases 1 cm.H2O lung volume will expand
200 ml.
- The diagram which shows the relation between lung volume
change and change in transpulmonary pressure refers to compliance diagram. (Figure
9.9).
- Compliance diagram shows two curves for expiration and
inspiration.
Total lung compliance, TLC: total lung capacity, FRC: functional residual capacity, RV: residual volume
Pulmonary surfactant
- Surfactant is a surface tension lowering agent present in
the alveolus between the alveolar fluid and air.
- It is a complex mixture of phospholipids (dipalmitoyl phosphocholine), proteins
and Ca2+.
- It is secreted by type
II alveolar epithelial cells which are 10% of the surface area of the
alveoli.
- Role of surfactant :
- Surfactant reduces surface
tension. The surface tension of normal fluid lining the alveoli without
surfactant is 50 dynes/cm, while
that for fluid lining the alveoli with normal surfactant is about 5-30dynes/cm.
-
It reduces compliance
resistance of the lungs.
-
It maintains alveolar
stability .It prevents over distention or collapse (atelectasis) of the
alveoli. When there is increase in the diameter of the alveoli, during
inspiration, the number of surfactant molecules per unit area decreases and the
surface tension increases.
- Surfactant production is decreased by the effect of smoking, histamine and hypoxia while its production increases by hormonal effect (insulin, thyroid hormone and glucocorticoid hormone).
Clinical note: Absence of surfactant from the fluid lining the alveoli especially in some newborn babies known as respiratory distress syndrome of newborn babies (hyaline membrane disease), which is fetal if it is not treated .That is why the premature babies may be at risk if they are born before the 6 -7 months of gestation.
Alveolar ventilation
- Volume of air moves in and out of the lungs with each normal
breath .This represents the tidal volume
(VT).The typical VT is about 500ml.
- There are 12-15 breathes per minute ,therefore the total air volume leaving the lung per minute (minute ventilation ) ,which is measured as in the following equation :
Minute
ventilation= respiratory rate X VT
= 12 breathes /min X 500 ml
= 6000 ml/min
Not all the air that passes the lips reaches the alveolar gas compartment ,where the gas exchange occurs, but about 150 ml remains behind in the anatomical dead space .So the alveolar ventilation (air volume entering g the respiratory zone ) is calculated as in the following equation;
Alveolar ventilation (AV) =12 breathes /min X( 500 ml _150ml )
= 4.2 Lit/minute
- Alveolar ventilation represents the fresh inspired air for gas exchange.
Lung volume and capacities
Overview
- The way to study the pulmonary ventilation is known spirometry, which is done by recording
the volume of air moved into and out of the lungs. The device which is used to
study the lung volumes is the spirometer,
while the record is the spirogram.
- Lung volumes and capacities are divided into two types
1. Static lung volumes and capacities
2. Dynamic lung volumes and
capacities.
- There are normal physiological differences in lung volumes and capacities, e .g; they are less in women than those in men in about 20-25%.They are greater in large and athletic people than in small asthenic people.
Clinical note: Lung volumes tend to decease in restrictive lung diseases (e.g., pulmonary fibrosis )
because of limitations of pulmonary expansion and they tend
to increase in obstructive
lung diseases (e.g., emphysema)
as a result of
Static lung volumes and capacities (figure 9.10)
§ Static lung volumes are not changed with time. They include
the following :
1-
The tidal volume (TV): The volume of air inspired or
expired with each normal breath (500ml).
2-
The Inspiratory Reserve Volume (IRV):
The
extra air volume that can be inspired forcefully after inspiration of normal
tidal volume.(3000 ml).
3-
The Expiratory Reserve Volume (ERV): The extra
amount of air that can be expired forcefully after the end of normal tidal
expiration.(1100ml).
4-
The Residual Volume (RV): Air volume remaining in the lungs
after the most forceful expiration. (1200ml).
Two or more of these volumes together are called: pulmonary capacities.
1- The Inspiratory Capacity(IC): amount of air that can be breathed beginning at the normal expiratory level and distending the lung to the maximum amount (3500ml).
2-
The functional Residual Capacity (FRC): amount of
air remaining in the lungs at the end of normal expiration. (2300ml).
FRC=RV+ERV
3-
Vital Capacity (VC): maximum amount of air that can be
expelled from the lung after first filling the lungs to their maximum extent
then expiring to the maximum extent. (4600ml).
VC=TV+IRV+ERV
4- The Total Lung Capacity (TLC): The maximum volume which lungs can be expanded with the greatest possible inspiratory effort.(5800 ml).
TLC=TV+IRV+ERV+RV
TLC=VC+RV
Clinical note: There are two
major categories of respiratory diseases, which can
alter the dynamic lung volumes:
Chronic Obstructive Pulmonary
Diseases (COPD): the diseases that interfere with
airflow. They are characterized by increased airway resistance to air flow caused by excessive secretion
or increased contraction of bronchial smooth muscle.
Asthma: is a disease
characterized by increased constriction of the bronchi and
bronchioles in response to various stimuli causing air narrowing and decrease
ventilation efficiency. The symptoms include rapid shallow breathing wheezing,
cough and shortness of breath.
Chronic bronchitis: is the
inflammation of the bronchioles causing swelling of the walls of
the bronchioles and bronchi and reducing air passage through them.
Emphysema results in damage to the
alveoli, so that the walls become less elastic (taking longer to inflate
and deflate).
Chronic Restrictive Pulmonary Disease (CRPD): is a chronic disorder that causes a decrease in lung’s ability to expand. It is characterized by reduced lung volume. The most common restrictive lung diseases are interstitial lung fibrosis including sarcoidosis granulomatous disorder and extrapulmonary restrictive lung diseases including scoiliosis.
Dynamic lung volumes
Dynamic lung
volumes quantify the time rate of gas flow along the airways.
They are of a clinical importance in the assessment of
airways resistance,
specifically
during expiration, therefore they are of interest in patients with
COPD like :asthma ,emphysema ,chronic
bronchitis .These are:
1-
Forced Vital Capacity (FVC): The maximum air volume which can be
expired forcefully after maximum inspiration.(Figure 9.11
).
2- Forced Expiratory Volume at the first second of expiration
(FEV1):
Maximum air volume which can be expired forcefully at the first second
of expiration after maximal inspiration.
3- FEV1%: Is the ratio of air expired forcefully at the first
second related
as a percentage of total amounts of air expired during
FVC.
FEV1%=FEV1/FVC X 100
4- Peak Expiratory Flow (PEF): is the maximal flow rate which is
achieved during force expiration. (Figure 9.11).
5- Maximum Voluntary Ventilation (MVV): is the maximal
air volume
which can be expired by breathing deeply and rapidly with maximal voluntary effort for a short time.
6- Forced Expiratory Time (FET): is the time
required to expire all air in
the lung by using the force.
7- Estimated Lung Age: is the age when
the person pulmonary function is
normal.
a: Expiratory flow curve showing PEF
,b: expiratory volume to showing FEV1and FVC
Pathology note:
FEV1
and FVC are reduced in lung diseases and the degree of reduction depends
on the nature of the diseases. In obstructive diseases the expiratory volumes
are reduced because of airway narrowing, therefore FEV1 is reduced more than is
FVC and FEV1% is reduced. In restrictive diseases, inspiration is
limited by noncompliance of the lung leading to limited expiratory volumes.
FVC is reduced more than is FEV1 resulting normal FEV1% or even increased,
because the elastic recoil of the lung is preserved.
Gas exchange
Overview
Gas exchange
across the respiratory membrane occurs by diffusion.
Respiratory gases
diffuse from area of high partial pressure to area of low
pressure.
Partial pressure: is the pressure
of each gas alone, which is used to express
the concentration of the gas.
- Partial pressure of O2 and CO2 are designed as PO2 and PCO2
respectively
- Partial pressure of a
gas is calculated by multiplying its fractional
concentration by the total pressure, for example the percentage of O2
is 21% of the total pressure 760 mmHg (atmospheric pressure), therefore
thePO2 is 160 mmHg
Atmospheric air ,alveolar air and expired air have
different concentrations of
gases because:
1-
Air is humidified before it reaches the alveoli.
2- A
constant diffusion of O2 from the alveoli into the blood, while CO2 is
constantly diffusing from the pulmonary blood to the
alveoli.
Diffusion of gases through the respiratory membrane
There are about
300 millions alveoli in the two lungs.
The alveolar walls are thin ,within them is a solid
network of
interconnecting capillaries, and blood flows in the
alveolar walls as a sheet Gas exchange
occurs through the membrane of all the terminal portions of
the lungs (not only the alveoli).These membranes are known
the respiratory membrane or the pulmonary membrane.
Respiratory membrane
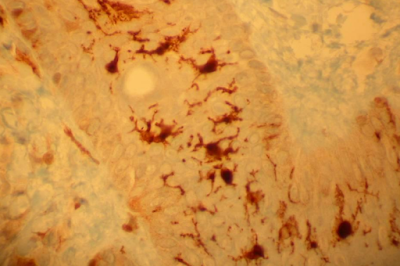
The respiratory
membrane is composed of the following layers(figure9.12):
1- A layer of fluid lining the alveoli that contains
surfactant.
2- The alveolar
epithelium
3- An epithelial basement membrane.
4- A thin interstitial space between the alveolar epithelium
and the
capillary membrane.
5- A capillary basement membrane
that, in many places, fuses with
epithelial basement membrane.
6- The capillary endothelial
membrane.
The membrane is
very thin, about 0.6 µm as average, and total surface area
is70 m2 in
normal adult .The total amount of blood in the lung capillaries is 60-140 ml, therefore the gas exchange is very
rapid.
The diameter of
pulmonary capillaries is 5 µm, so the RBCs must squeeze
through them (RBC
touches the membrane) and O2, CO2 dot
need to pass
through the plasma.
Factors affecting the rate of diffusion through
the respiratory
membrane
1- The thickness of the membrane.
2- The surface area of the membrane.
3- The diffusion coefficient of the gas in the substance of the membrane.
4- The pressure differences between the two sides of
the membrane.
The respiratory membrane
Diffusing capacity of the respiratory membrane
Diffusing capacity is the volume of gas that is able to
diffuse across the
respiratory membrane in 1 minute with pressure gradient across the membrane of 1 mmHg.
Exchange of O2 is normally so efficient that is perfusion
limited (the
amount of O2 that enters the arterial circulation is
limited only by the
amount of blood flow to the lung).
The diffusing
capacity of the lung for CO2 is 20 times greater than that for
O2.At rest the diffusing capacity for O2 is 21ml/min/mmHg, while its 440ml /min/mmHg for CO2.
All factors that
affect diffusion through the respiratory membrane can affect
the diffusing capacity.
The diffusing
capacity for O2 increases during exercise.
Perfusion -limited and diffusion-limited gas exchange
Perfusion -limited gas exchange: diffusion can be
increased only if blood
flow increases, e.g., O2 uptake under normal condition.
Diffusion- limited exchange: diffusion continues as long
as pressure
differences exist
across the respiratory membrane, e.g., O2 diffusion during
heavy exercise at high altitude.
Pulmonary blood flow
The pressures in
the pulmonary circulation are low compared with those of
systemic circulation.
In the upright
position ,perfusion in the apices of the lung is different from
that of the bases
because the effects of gravity, therefore there are three
zones of pulmonary blood flow:
1-
Zone 1(top of the lung)
It has no blood flow because alveolar pressure is greater than artery
pressure.
It can occur when
pulmonary artery pressure is decreased
(hemorrhage) and when alveolar pressure is increased.
Disclaimer:
The
content provided in this article is based on personal knowledge and
educational background in the fields of health and nutrition. It is
intended for informational purposes only and should not be considered a
substitute for professional medical advice. For any health concerns,
please consult a qualified healthcare provider .










Comments
Post a Comment